The Foreign Objects manage to make their way into the human body. “Foreign objects“ are items that (POISONING, BITES, STINGS) enter the body through a wound in the skin or an orifice. These might range from grit in the eye to little things pushed into young children’s noses and ears.
These can be distressing but do not usually cause serious problems for the casualty. Poisoning may result from exposure to or ingestion of toxic substances, chemicals, and contaminated food.
Effects of poisons vary but medical advice will be needed in most cases, Insect stings and marine stings can often be treated with first aid.
However, multiple stings can produce a reaction that requires urgent medical help. Animal and human bites always require medical attention due to the risk of infection.
AIMS AND OBJECTIVES
- To ensure the safety of yourself and the casualty.
- To assess the casualty’s condition quickly and calmly.
- To assess the potential d foreign Object.
- To identify the poisonous substance.
- To comfort and reassure the casualty.
- To took tor of and treat any injuries associated With the condition.
- To obtain medical help if necessary Call 999/1 12 for emergency help if you suspect a serious illness or injury.
- To be aware Of your Own needs.
Foreign Objects: THE SENSORY ORGANS
THE SKIN
The skin covers and protects the human body. This is one of the body’s major organs, with two layers: the epidermis (outer layer) and the dermis (inner layer).
The dermis is the innermost layer. The skin acts as a barrier against pathogens and hazardous substances. It is also a vital sense organ, as it contains nerves that allow the body to detect heat, cold, pain, and touch.
Structure of the skin
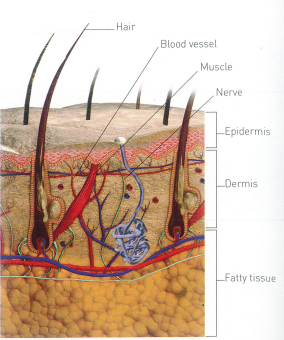
The skin consists of the thin epidermis and the thicker dermis. Which sit on a layer of fatty tissue (subcutaneous fat), Blood vessels. nerves. muscles, sebaceous (oil) glands. sweat glands and hair roots (follicles) lie in the dermis.
THE EYES
These complex organs enable us to see the world around us. Each eye consists of a colored part (iris) with a small opening (pupil) that allows rays of light to enter the eye.
The size of the pupil changes according to the amount of light that is entering the eye. Light rays are focused by the transparent lens onto a “screen” (retina) at the back of the eye.
Special cells in the retina convert this information into electrical impulses that then travel, via the optic nerve that leads from the eye to the part of the brain where the impulses are analyzed.
Each eye is protected by a bony socket in the skull. The eyelids and delicate membranes called conjunctiva protects the front of the eyes.
Tears form a protective film across the front of the conjunctiva. lubricating the surface and flushing away dust and dirt.
Structure of the EYE
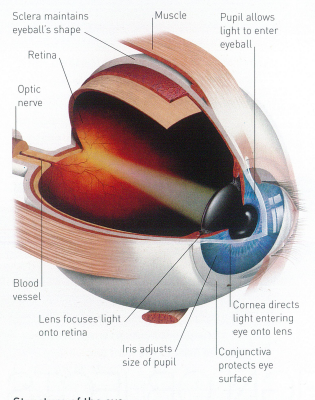
The eyes are fluid-filled. spherical structures about 28cm, diameter They have focusing parts (cornea and lens). and light- and color-sensitive cells in the retina.
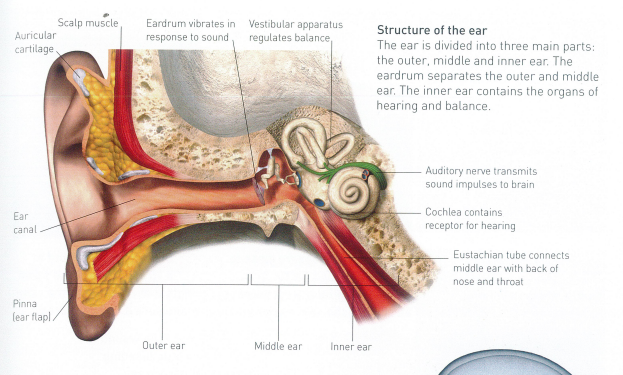
THE EARS
As well as being the organs of hearing, the ears also play an important role in balance. The visible part of each ear, the auricle, funnels sounds into the ear canal to vibrate the eardrum, Fine hairs in the ear canal filter out dust, and glands secrete ear wax to trap any other small particles.
The vibrations of the eardrum pass across the middle ear to the hearing apparatus [cochlea] in the inner ear. This structure converts the vibrations into nerve impulses and transmits them to the brain via the auditory nerve The vestibular apparatus within the inner ear is involved in balance.
Structure of the ear
THE MOUTH AND NOSE
These cavities form the entrances to the digestive and respiratory tracts respectively The nasal cavities connect with the throat.
They are lined with blood vessels and membranes that secrete mucus to trap debris as it enters the nose.
Food enters the digestive tract via the mouth, which leads into the gullet (esophagus) the epiglottis. a flap at the back of the throat. prevents food from entering the windpipe (trachea).
Structure Of the mouth and nose
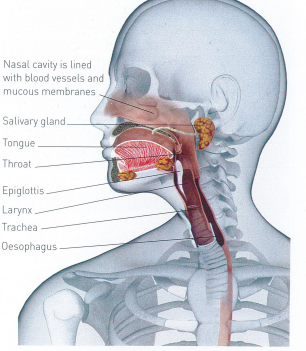
The nostrils lead into the two nasal cavities. Which are lined with mucous membranes and blood vessels.
The nasal cavities connect directly with the top of the throat. which is at the back of the mouth.
Foreign Objects: SPLINTER
Small splinters of wood, metal, or glass may enter the skin They carry a risk of infection because they are rarely clean Often a splinter can be successfully withdrawn from the skin using a tweezer.
If the splinter is severely embedded, though. lays on top of a joint You should leave it in place and encourage the casualty to seek medical help if it is difficult to remove.
YOUR AIMS
- To remove the splinter.
- To minimize the risk of infection.
CAUTION
Ask the casualty about tetanus immune satiam Seek medical advice if he has a dirty wound; he has never been immunized: he is uncertain about the number and timing of injections; he has not had at least five injections previously.
- Gently clean the area around the splinter with soap and warm water.
2. Hold the tweezers close to the end for a better grip. Grasp the splinter with tweezers as close to the skin as possible.

3. Draw the splinter out in a straight line at the same angle that it went into the skin; make sure it does not break.

4. Carefully squeeze the wound to encourage a little bleeding. This will help to flush out any remaining dirt.

5. Clean and dry the wound and cover it with a dressing.
SPECIAL CASE EMBEDDED SPLINTER
If a splinter is embedded or difficult to dislodge. do not probe the area with a sharp object, such as a needle or you may introduce infection, Pad around the splinter until you can bandage over it without pressing on it, and seek medical help.
Foreign Objects: EMBEDDED FISH-HOOK
A fish hook that is embedded in the skin is difficult to remove because of the barb at the end of the hook.
If at all feasible, you should get the hook removed by a medical practitioner. If medical assistance is unavailable, only attempt to remove a hook yourself.
Fish hooks embedded in the skin can cause illness, even tetanus.
What are the YOUR AIMS?
- To obtain medical help
- To minimi5e the risk of infection.
- lf help is delayed, remove the fish-hook without causing the casualty any further injury and pain.
Be CAUTION
- Do not try to pull out a fish- hook unless you can cut off the barb. If you cannot. seek medical help,
- Ask the casualty about tetanus immunisation_ Seek medical advice if, he has a dirty wound; he has never been immunised; he is uncertain about number and timing of injections; he has not had at least five injections previously.
- Support the injured area. If possible, cut off the fishing line as close to the hook as possible.
2. If medical help is readily available, build-up pads of gauze around the hook until you can bandage over the top without pushing it in further. Bandage over the padding and the hook and arrange to take or send the casualty to the hospital.

3. If medical help is unavailable, you can try to remove the hook. If the barb is visible, use wire cutters to cut it away; then carefully withdraw the hook back through the skin by its eye.

4. Clean and dry the wound and cover it with a dressing.
SPECIAL CASE IF BARB IS NOT VISIBLE
If the barb is embedded in the skin, gently move the hook forward until it emerges. Cut the barb as described in step 3 above.
Then take the hook by the eye and pull it out. If you can’t get the barb out, wrap a pad around the hook, secure it with a bandage, and get medical care as quickly as possible.
FOREIGN OBJECT IN THE EYE
Foreign objects such as grit. a loose eyelash or a contact lens floating on the eye’s surface can easily be rinsed out.
However, you must not attempt to remove anything that sticks to the eye or penetrates the eyeball because this may damage the eye. Instead, make sure that the casualty receives urgent medical attention.
How to RECOGNITION?
- Blurred vision;
- Pain or discomfort;
- Redness and watering of the eye;
- Eyelids screwed up in spasm.
What are the YOUR AIMS?
- To prevent injury to the eye.
Be CAUTION
- Do not touch anything that is sticking to. or embedded in. the eyeball Cover the eye and arrange to take or send casualty to hospital.
- Advise the casualty not to rub her eye. Ask her to sit down facing a light.
2. Stand beside, or just behind, the casualty. Gently separate her eyelids with your thumbs or finger and thumb. Ask her to look right, left, up, and down. Examine every part of her eye as she does this.

3. If you can see a foreign object on the white of the eye. wash it out by pouring clean water from a glass or jug, or by using a sterile eyewash if you have one.
Put a towel around the casualty’s shoulders. Hold her eye open and pour the water from the inner corner so that it drains onto the towel.
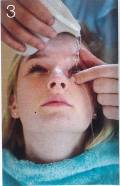
4. If this is unsuccessful, try lifting the object off with a moist swab or the damp corner of a clean handkerchief or tissue. If you still cannot remove the object, seek medical help.
SPECIAL CASE IF OBJECT IS UNDER UPPER EYELID
Ask the casualty to grasp the lashes on her upper eyelid and pull the upper lid over the lower lid; the lower lashes may brush the particle clear.
If this is unsuccessful, ask her to try blinking underwater since this may also make the object float off, Do not attempt to do this if the object is large or abrasive.
FOREIGN OBJECT IN THE EAR
If a foreign object becomes lodged in the ear, it may cause temporary deafness by blocking the ear canal. In some cases, a foreign object may damage the eardrum.
Young children frequently push objects into their ears. The tips of cotton wool buds are often left in the ear. Insects can fly or crawl into the ear and may cause distress.
What are the YOUR AIMS?
- To prevent injury to the ear.
- To remove a trapped insect
- To arrange transport to hospital if a foreign object is lodged in the ear.
Be CAUTION
- Do not attempt to remove any object that is lodged in the ear. You may cause serious injury and push the foreign object in further.
- Arrange to take or send the casualty to hospital as soon as possible. Do not try to remove a lodged foreign object yourself.
2. Reassure the casualty during the journey or until medical help arrives.
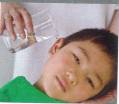
SPECIAL CASE INSECT INSIDE THE EAR
Reassure the casualty and ask him to sit down. Support his head. with the affected ear uppermost. Gently flood the ear with tepid water; the insect should float out. If this flooding does not remove the insect, seek medical help.
FOREIGN OBJECT IN THE NOSE
Young children may push small objects up their noses. Objects can block the nose and cause infection.
If the object is sharp it can damage the tissues, and “button” batteries can cause burns and bleeding, Do not try to remove a foreign object: you may cause injury or push it further into the airway.
How to RECOGNITION?
- Difficult or noisy breathing through the nose;
- Swelling of the nose:
- Smelly or blood-stained discharge, indicating that an object may have been lodged for a while.
What the YOUR AIMS?
- To arrange transport to hospital.
Be CAUTION
- Do not attempt to remove the foreign object, even if you can see it.
- Try to keep the casualty quiet and calm. Tell him to breathe through his mouth at a normal rate. Advise him not to poke inside his nose to try to remove the object himself.
2. Arrange to take or send the casualty to the hospital to safely remove it by medical staff.
HOW POISONS AFFECT THE BODY
A poison (toxin) is a substance that, if taken into or absorbed into the body in sufficient quantity, can cause either temporary or permanent damage.
Poisons can be swallowed, absorbed through the skin, inhaled, splashed into the eyes, or injected. Once in the body, they may enter the bloodstream and be carried swiftly to all organs and tissues, Signs and symptoms of poisoning vary with the poison.
They may develop quickly or over several days. Vomiting is common, especially when the poison has been ingested. Inhaled poisons often cause breathing difficulties.
TYPES OF POISON
Some poisons are man-made – for example, chemicals and drugs – and these are found in the home as well as in industry.
Almost every household contains potentially poisonous substances, such as bleach and paint stripper, as well as prescribed or over-the-counter medicines, which may be dangerous if taken In excessive amounts.
Other poisons occur in nature: plants produce poisons that may irritate the skin or cause more serious symptoms if ingested, and various insects and creatures produce venom in their bites and stings.
Contamination of food by bacteria may result in food poisoning – one of the most common forms of poisoning.
RECOGNISING AND TREATING THE EFFECTS OF POISONING
| ROUTE OF ENTRY INTO THE BODY | POISON | POSSIBLE EFFECTS | ACTION |
| Swallowed (ingested) | • Drugs and alcohol • Cleaning products • DIY and gardening products • Plant poisons • Bacterial food poisons • Viral food poisons | • Nausea and vomiting • Abdominal pain • Seizures • Irregular, or fast, or slow. heartbeat • Impaired consciousness | • Monitor casualty • Call emergency help • Commence CPR if necessary • Use a face mask to protect yourself if you need to give rescue breaths |
| Absorbed through the skin | • Cleaning products • DIY and gardening products • Industrial poisons • Plant poisons | • Swelling • Rash • Redness • Itching | • Remove contaminated clothing • Wash with cold water for 20 minutes • Seek medical help • Commence CPR if necessary |
| Inhaled | • Fumes from cleaning and DIY products • Industrial poisons • Fumes from fires | • Difficulty breathing • Hypoxia • Grey-blue skin (cyanosis) | • Help casualty into the fresh air • Call emergency help • Commence CPR if necessary |
| Splashed in the eye | • Cleaning products • DIY and gardening products • Industrial poisons • Plant poisons | • Pain and watering of the eye • Blurred vision • Pain. redness and swelling at the injection site • Blurred vision | • Irrigate the eye for ten minutes • Call emergency help • Commence CPR if necessary For sting/venom: |
| Injected through the skin | • Venom from stings and bites • Drugs | • Nausea and vomiting • Difficulty breathing • Seizures • Impaired consciousness • Anaphylactic shock | • Remove sting, if possible • Call emergency help • Commence CPR if necessary For injected drugs: • Call emergency help • Commence CPR if necessary |
SWALLOWED POISONS
Chemicals that are swallowed may harm the digestive tract, or cause more widespread damage if they enter the bloodstream and are transported to other parts of the body Hazardous chemicals include household substances such as bleach and paint stripper, which are poisonous or corrosive if swallowed Drugs, both prescribed or those bought over the counter, can also be harmful if an overdose is taken. Some plants and their berries can also be poisonous.
How to RECOGNITION?
- History of ingestion/ exposure.
- Depending on what has been swallowed, there may be:
- Vomiting. sometimes bloodstained, later diarrhea:
- Cramping abdominal pains;
- Pain or a burning sensation;
- Empty containers in the vicinity;
- Impaired consciousness:
- Seizures.
What are the YOUR AIMS?
- To maintain an open airway. breathing and circulation.
- To remove any contaminated clothing.
- To identity the poison.
- To arrange urgent removal to hospital.
- If the casualty is conscious, ask her what she has swallowed, and if possible how much and when. Look for clues – for example, poisonous plants, berries, or empty containers. Try to reassure her.
2. Call 999/112 for emergency help. Give ambulance control as much information as possible about the poison. This information will assist the medical team to treat the casualty.

3. Monitor and record the casualty’s vital signs while waiting for help to arrive. Keep samples of any vomited material. Give these samples. containers and any others clues to the ambulance crew.
DRUG POISONING
Poisoning can result from an overdose of prescribed drugs, or drugs that are bought over the counter. It can also be caused by drug abuse or drug interaction.
The effects vary depending on the type of drug and how it is taken (below). When you call the emergency services, give as much information as possible.
While waiting for help to arrive. look for containers that might help you to identify the drug.
What are the YOUR AIMS?
- To maintain breathing and circulation.
- To arrange removal to hospital.
Be CAUTION
- Do not induce vomiting.
- If the casualty loses consciousness. open the airway and check breathing.
- If the casualty is conscious. help him into a comfortable position and ask him what he has taken. Reassure him while you talk to him call 999/112.
- For emergency help Tell ambulance control you suspect drug poisoning. Monitor and record vital signs level of response, breathing and pulse while waiting for help to arrive.
- Keep samples of any vomited material. Look for evidence that might help to identify the drug. such as empty containers. Give these samples and containers to the ambulance personnel.
RECOGNISING THE EFFECTS OF DRUG POISONING
| CATEGORY | DRUG | EFFECTS OF POISONING |
| Painkillers | • Aspirin (swallowed) • Paracetamol (swallowed) | • Upper abdominal pain. nausea and vomiting • Ringing in the ears • Sighing” when breathing • Confusion and delirium • Dizziness |
| Nervous system depressants and tranquillisers | • Barbiturates and benzodiazepines (swallowed) | • Little effect at first. but abdominal pain. nausea and vomiting may develop • Irreversible liver damage may occur within three days lalcohol and malnourishment increase the (risk) |
| Stimulants and hallutinogens | • Amphetamines (including ecstasy) and LSD (swallowed) • Cocaine (inhaled or injected) | • Lethargy and sleepiness, leading to unconsciousness •Shallow breathing • Weak. irregular or abnormally slow Or fast pulse |
| Narcotics | • Morphine. heroin (commonly injected) | • Excitable. hyperactive behaviour, agitation • Sweating • Tremor of the hands • Hallucinations. in which the casualty may claim to “hear voices” or see things” • Dilated pupils |
| Solvents | • Glue, lighter fuel (inhaled) | • Small pupils •Sluggishness and confusion. possibly leading to unconsciousness • Slow. shallow breathing, which may stop altogether • Needle marks. which may be infected |
| Anaesthetic | • Ketamine DRUG | • Nausea and vomiting • Headaches • Hallucinations • Possibly, unconsciousness • Rarely. cardiac arrest • Drowsiness • Shallow breathing •Hallucinations |
ALCOHOL POISONING
Alcohol (chemical name: ethanol) is a drug that depresses the activity of the central nervous system -in particular the brain. Prolonged or excessive intake can severely impair all physical and mental functions, and the person may sink into deep unconsciousness.
There are other risks to a casualty from alcohol poisoning for example: an unconscious casualty may inhale and choke on vomit; alcohol widens (dilates) the blood vessels so the body loses heat, and hypothermia may develop A casualty who smells of alcohol may be misdiagnosed and not receive appropriate treatment for an underlying cause of unconsciousness, such as a head injury, stroke. heart attack or hypoglycaemia.
How to RECOGNITION?
- A strong smell of alcohol;
- Empty bottles or cans:
- Impaired consciousness: the casualty may respond if roused, but will quickly relapse;
- Flushed and moist face;
- Deep, noisy breathing;
- Full, bounding pulse;
- Unconsciousness. In the later stages of unconsciousness:
- Shallow breathing;
- Weak, rapid pulse;
- Dilated pupils that react poorly to Light.
What are the YOUR AIMS?
- To maintain an open airway.
- To assess for other conditions.
- To seek medical help if necessary.
Be CAUTION
- Do not induce vomiting.
- If the casualty loses consciousness. open the airway and check his breathing.
- Cover the casualty with a coat or blanket to protect him from the cold.

2. Assess the casualty for any injuries, especially head injuries, or other medical conditions.
3. Monitor and record vital signs level of response, pulse and breathing until the casualty recovers or is placed in the care of a responsible person. If you are in any doubt about the casualty’s condition: call 999/112 for emergency help.
ANIMAL AND HUMAN BITES
Bites from sharp, pointed teeth cause deep puncture wounds that can damage tissues and introduce germs. Bites also crush the tissue, Any bite that breaks the skin needs prompt first aid because of the increased risk of infection.
A serious infection risk is rabies, a potentially fatal viral infection of the nervous system. The virus is carried in the saliva of infected animals, If bitten in an area where there is a risk of rabies, seek medical advice since the casualty must be given anti-rabies injections. Try to identify the animal. Tetanus is also a potential risk following any animal bite.
There is probably only a small risk of hepatitis viruses being transmitted through a human bite – and an even smaller risk of transmission of the HIV/AIDS virus. However. medical advice should be sought straight away.
What are the YOUR AIMS?
- To control bleeding.
- To minimise the risk of infection,
- To obtain medical help if necessary.
CAUTON
- lf you suspect rabies, arrange to take or send the casualty to hospital immediately.
- Ask the casualty about tetanus immunisation. Seek medical advice if he has a dirty wound; he has never been immunised; he is uncertain about the number and timing of injections, he has not had at least five injections previously.
- Wash the bite wound thoroughly with soap and warm water in order to minimise the risk of infection.
2. Raise and support the wound and pat dry with clean gauze swabs. Then cover with a sterile wound dressing.

3. Arrange to take or send the casualty to hospital if the wound is large or deep.
SPECIAL CASE: FOR A DEEP WOUND
If the wound is deep. control bleeding by applying direct pressure over a sterile pad and raise the injured part, Cover the wound and pad with a sterile dressing or large, clean non-fluffy pad and bandage firmly in place. Treat the casualty for shock and call 999/112 for emergency help.
INSECT STING
Usually, a sting from a bee, wasp or hornet is painful rather than dangerous. An initial sharp pain is followed by mild swelling, redness and soreness. However, multiple insect stings can produce a serious reaction.
A sting in the mouth or throat is potentially dangerous because swelling can obstruct the airway. With any bite or sting, it is important to watch for signs of an allergic reaction, which can lead to anaphylactic shock. Such reactions account for about ten deaths a year in the UK.
How to RECOGNITION?
- Pain at the site of the sting.
- Redness and swelling around the site of the sting.
What are the YOUR AIMS?
- To relieve swelling and pain.
- To arrange removal to hospital if necessary.
CAUTION
Call 999/112 for emergency help if the casualty shows signs of anaphylactic shock such as breathing difficulties and/or swelling of the face and neck.
Monitor and record vital signs – level of response. breathing and pulse – while waiting for help to arrive.
- Reassure the casualty. If the sting is visible, brush or scrape it off sideways with the edge of a credit card or your fingernail. Do not use tweezers because you could squeeze the sting and inject more poison into the casualty.

2. Raise the affected part if possible, and apply a cold compress such as an ice pack to minimise swelling. Advise the casualty to keep the compress in place for at least ten minutes. Tell her to seek medical advice if the pain and swelling persist.

3. Monitor vital signs – level of response, breathing and pulse Watch for signs of an allergic reaction, such as wheezing.
SPECIAL CASE: STINGS IN THE MOUTH AND THROAT
If a casualty has been stung in the mouth, there is a risk that swelling of tissues in the mouth and/or throat may occur, causing the airway to become blocked.
To help prevent this. give the casualty an ice cube to suck or a glass of cold water to sip. Call 999/112 for emergency help if swelling starts to develop.
OTHER BITES AND STINGS
Bites from certain species of scorpion, spider and mosquito can cause serious illness, and may even be fatal if not treated promptly.
Bites or stings in the mouth or throat are dangerous because swelling can obstruct the airway. Be alert to an allergic reaction. which may Lead the casualty to suffer an anaphylactic shock.
How to RECOGNITION?
Depends on the species, but generally:
- Pain, redness and swelling at site of sting:
- Nausea and vomiting:
- Headache.
What are the YOUR AIMS?
- To relieve pain and swelling.
- To arrange removal to hospital if necessary.
CAUTION
Call 999/112 for emergency help if a scorpion or a red back or funnel web spider has stung the casualty. or if the casualty is showing signs of anaphylactic shock.
TICK BITE
Ticks are tiny, spider-like creatures found in grass or woodlands. They attach themselves to passing animals (including humans] and bite into the skin to suck blood.
When sucking blood, a tick swells to about the size of a pea. and it can then be seen easily. Ticks can carry disease and cause infection, so they should be removed as soon as possible.
What are the YOUR AIMS?
- To remove the tick.
CAUTION
- Do not try to remove the tick with butter or petroleum jelly or burn or freeze it. since it may regurgitate infective fluids into the casualty.
- Using tweezers, grasp the tick’s head as close to the casualty’s skin as you can. Pull the head upwards using steady even pressure. Do not use twisting or jerking movements as this may leave mouth parts embedded, or cause the tick to regurgitate infective fluids into the skin.

2. Save the tick for identification; place it in a sealed plastic bag. The casualty should seek medical advice; tell him to take the tick since it may be required for analysis.
SNAKE BITE
Snake bites are uncommon in the UK. The only poisonous snake native to mainland Britain is the adder, and its bite is rarely fatal.
However, poisonous snakes are sometimes kept as pets People are also exposed to venomous snakes through travel. While a snake bite is not usually serious, it is safer to assume that a snake is venomous.
A venomous bite is often painless. Depending on the snake, venom may cause local tissue destruction. it may spread, blocking nerve impulses, causing heart and breathing to stop or it can cause blood clotting (coagulation) and then internal bleeding.
Note the time of the bite, as well as the snake’s appearance to help doctors identify the correct antivenom Take precautions to prevent others being bitten. Notify the authorities who will deal with the snake.
How to RECOGNITION?
There may be:
- A pair of puncture marks – the bite may be painless;
- Severe pain, redness and swelling at the bite;
- Nausea and Disturbed vision;
- Increased salivation and sweating:
- Laboured breathing; it may stop altogether,
What are the YOUR AIMS?
- To prevent venom spreading.
- To arrange urgent removal to hospital.
CAUTION
- Do not apply a tourniquet, slash the wound with a knife or try to suck out the venom.
- If the casualty loses consciousness, open the airway and check breathing.
- Help the casualty to lie down, with head and shoulders raised. Reassure the casualty, tell her to keep calm and advise her not to move her limbs. Call 999/112 for emergency help.
2. If there is no pain, apply a pressure bandage at the site of the bite. Do not remove clothing from around the site since this can speed up the absorption of the venom.

3. Apply another pressure bandage to extend from the bite as far up the limb as possible. Tie it as for a sprained ankle, and check circulation after bandaging. If possible, mark the site of the bite. Immobilise the limb by securing it to the other leg with broad- and narrow-fold bandages.

4. Monitor and record vital signs while waiting for help to arrive. The casualty needs to remain still.
STINGS FROM SEA CREATURES
Jellyfish, Portuguese men-of-war, sea anemones and corals can all cause stings. Their venom is contained in stinging cells that stick to the skin.
Most marine species found in temperate regions of the world are not dangerous.
However, some tropical marine creatures can cause severe poisoning. Occasionally, death results from paralysis of the chest muscles and, very rarely, from anaphylactic shock.
How to RECOGNITION?
Depends on the species, but generally: Pain, redness, and swelling at the site of the sting;
- Nausea and vomiting;
- Headache
What are the YOUR AIMS?
- To relieve pain and discomfort.
- To seek medical help if necessary.
CAUTION
- If the injury is extensive or there is a severe reaction, call 999/112 for emergency help. Monitor and record vital signs – level of response. breathing and pulse while waiting for help to arrive.
- Encourage the casualty to sit or lie down. Immerse the affected area in hot water (40-410C/104-1060F) for ten minutes to relieve pain and swelling.
2. Alternatively, wash the area in copious quantities of cold water.
3. Monitor vital signs – level of response, breathing, and pulse. Watch for signs of an allergic reaction, such as wheezing.
MARINE PUNCTURE WOUND
Many marine creatures have spines that provide a mechanism against attack from predators but that can also cause painful wounds if trodden on.
Sea urchins and weever fish have sharp spines that can become embedded in the sole of the foot. Wounds may become infected if the spines are not removed. Hot water breaks down fish venom.
What are the YOUR AIMS?
- To relive pain and discomfort.
CAUTION
- Do not bandage the wound.
- Do not scald the casualty,
- Help the casualty to sit down. Immerse the injured part in water as hot as he can tolerate for about 30 minutes.
2. Take or send the casualty to the hospital so that the spines can be safely removed.

