What are the common medical conditions?
Common Diseases, Many everyday medical conditions, like fever and headache, need prompt treatment and respond well to care. However. a minor complaint is often the beginning of a significant illness, so you ought to always be aware of this and seek medical conditions advice if you’re unsure about the casualty 5 conditions.
Other medical conditions like diabetes-related hypoglycemia than normal blood glucose levels). severe allergies (anaphylaxis) and meningitis are potentially life-threatening and need urgent medical attention.
Miscarriage, however, may be a potentially significant issue thanks to the danger of severe bleeding. A who is miscarrying needs urgent medical help.
List of common medical conditions and common diseases
- DIABETES MELLITUS
- HYPERGLYCAEMIA
- ALLERGY
- ANAPHYLACTIC SHOCK
- FEVER
- MENINGITIS
- HEADACHE
- MIGRAINE
- EARACHE AND TOOTHACHE
- SORE THROAT
- ABDOMINAL PAIN
- STITCH
- VOMITING AND DIARRHOEA
- HYPOGLYCAEMIA
Medical Conditions – DIABETES MELLITUS

This is a long-term (chronic) condition in which the body fails to produce sufficient insulin. Insulin is a chemical produced by the pancreas la gland that lies behind the stomach, which regulates the blood sugar (glucose) level in the body. This condition can result in higher-than-normal blood sugar (hyperglycemia) or lower than normal blood sugar hypoglycemia.
Here are medical conditions for If a person with diabetes is unwell, giving him sugar will rapidly correct hypoglycemia and is unlikely to do harm in cases of hyperglycemia referred to as juvenile diabetes or early-onset diabetes because it usually develops in childhood or teenage years. Insulin can be administered using a syringe or an injection pen [insulin pen). In some cases, it is given via a “pump”, a small device about the size of a pack of cards that is strapped to the body. The insulin is administered via a piece of tubing that leads from the pump to a needle that sits just under the skin.
TYPES OF DIABETES
There are two types:
Type 1, or insulin dependent diabetes, and sort 2, or type II diabetes. In Type 1 diabetes, the body produces little or no insulin. People with Type 1 diabetes need regular insulin injections throughout their lives. it’s sometimes
In Type 2 diabetes, the body doesn’t make enough insulin or cannot use it properly. this sort is typically linked with obesity and is additionally referred to as type II diabetes because it is more common in people over the age of 40. the danger of developing this sort is increased if it runs in your family Type 2 diabetes can normally be controlled with diet, weight loss, and regular exercise. However, oral medication and, in some cases, insulin injections could also be needed.
Medical Conditions – HYPERGLYCAEMIA
High blood glucose (hyperglycemia) develops slowly over a period of days. those that suffer from hyperglycemia may wear warning bracelets, cards, or medallions alerting a primary aider to the condition. If it’s not treated, hyperglycemia will end in unconsciousness [diabetic coma) then requires urgent treatment within the hospital.
Symptoms and How to recognizes
- Warm. dry skin.
- Rapid pulse and breathing.
- Fruity sweet breath and excessive thirst
- Drowsiness, leading to unconsciousness if untreated.
Caution:- If the casualty loses consciousness, open the airway and check breathing. (unconscious casualty)
What you can do:
- Call 999/112 for emergency help, tell ambulance control that you suspect hyperglycemia.
- Monitor and record vital signs – the level of response, breathing, and pulse.
Medical Conditions – HYPOGLYCAEMIA

This condition occurs when the blood glucose level falls below normal. it’s characterized by a rapidly deteriorating level of response Hypoglycaemia develops if the insulin-sugar balance 1s incorrect; for instance, when an individual with diabetes misses a meal or takes an excessive amount of exercise. it’s more common for a person with newly diagnosed diabetes while he’s becoming won’t to balancing sugar levels.
More rarely, hypoglycemia may develop following a convulsion or after an episode of binge drinking. It also can occur with heat prostration or hypothermia.
People with diabetes may carry their own blood-te kits to see their blood glucose levels, also as their insulin medication, so are well prepared for emergencies; for instance, many carry sugar lumps or a tube of glucose gel.
If the hypoglycaemic attack is at a complicated stage, consciousness could also be impaired and you want to seek emergency help.
Symptoms and How to recognizes
- A history of diabetes – the casualty may recognize the onset of a hypo attack himself.
- Weakness, faintness, or hunger.
- Confusion and irrational behavior.
- Sweating with cold, clammy skin.
- Rapid pulse.
- Palpitations and muscle tremors.
- Deteriorating level of response.
- Diabetic identity bracelet or necklace. glucose gel, medication such as tablets, or an insulin syringe.
What you can do:
- To raise the sugar content of the blood as quickly as possible
- To obtain appropriate medical help.
- Help the casualty to Sit down. Give him a sugary drink. Sugar lumps Or sweet food. If he has his own 0m glucose helps him to take it.
2. If the casualty responds quickly, give him more food or drink and let him rest until he feels better, Help him find his glucose testing kit so that he can check his glucose level. Monitor him until he is completely recovered.
3. If his condition does not possible causes. Call 999/112 for emergency help and monitor and vital signs of breathing and pulse, while waiting for help to arrive.
Caution:-
- If consciousness is impaired, do not give the casualty anything to eat or drink.
- If the casualty loses consciousness, open the airway and check to breathe. (unconscious casualty)
Medical Conditions – ALLERGY

An allergy is an abnormal reaction of the body’s defense system (immune response) to a normally harmless “trigger” substance [or allergen I. An allergy can happen as mild itching, swelling, wheezing, or digestive condition, or can reach full-blown anaphylaxis, or anaphylaxis (opposite). which may occur within seconds or minutes of exposure to an offending allergen.
Medical conditions of allergy, Common triggers include pollen, dust, nuts, shellfish, eggs, wasp and bee stings, latex, and certain medications. Skin changes are often subtle, absent, or variable in up to twenty percent of allergies.
Symptoms and How to recognizes
Features of mild allergy vary depending on the trigger and the person. There may be:
- Red, itchy rash or raised areas of skin (weals)
- Red, itchy eyes
- Wheezing and/or difficulty breathing
- Swelling of hands, feet, and/or face
- Abdominal pain, vomiting, and diarrhoea
What you can do:
- To assess the severity of the allergic reaction.
- To seek medical advice if necessary.
To do:
- Assess the casualty’s signs and symptoms. Ask if she has any known allergies.
2. Remove the trigger if possible, or move the casualty from the trigger.
3. Treat any symptoms. Allow the casualty to take her own medication for a known allergy.
4. If you are at all concerned about the casualty’s condition, seek medical advice.
Medical Conditions – ANAPHYLACTIC SHOCK
This is a severe allergy affecting the entire body. it’s going to develop within seconds or minutes of contact with a trigger and is potentially fatal. In an anaphylactic reaction, chemicals are released into the blood that widens (dilate) blood vessels.
This causes vital signs to fall and air passages to narrow [constrict]. leading to breathing difficulties. additionally, the tongue and throat can swell, obstructing the airway the quantity of oxygen reaching the vital organs are often severely reduced, causing hypoxia. Common triggers include nuts, shellfish, eggs, wasp and bee stings, latex, and certain medications.
A casualty with anaphylactic shock needs emergency treatment with an injection of adrenaline. (epinephrine)
Symptoms and How to recognizes
Features of allergy [opposite] may be present:
- Red, itchy rash or raised areas of skin [weals);
- Red itchy, watery eyes;
- Swelling of hands, feet, and/or face:
- Abdominal pain, vomiting, and diarrhoea.
There may also be:
- Difficulty breathing, ranging from a tight chest to severe difficulty, causing the casualty to wheeze and gasp for air.
- Pale or flushed skin.
- Visible swelling of tongue and throat with puffiness around the eyes.
- The feeling of terror.
- Confusion and agitation.
- Signs of shock, leading to collapse and loss of consciousness.
What you can do:
- To ease breathing.
- Treat shock.
- To arrange urgent removal to hospital.
To do:
- Check whether the casualty is carrying any medication -a syringe or an auto-injector of adrenaline (epinephrine] -and help her to use it. If she is unable to administer it, and you have been trained to use an autoinjector, you may give it to her. Pull off the safety cap and, holding the injector with your fist, place the tip firmly against the casualty’s thigh to release the medication lit can be delivered through clothing).
2. Help the casualty to sit up in the position that best relieves any breathing difficulty. If she becomes pale with a weak pulse, help her to lie down with legs raised and treat tor shock.

3. Monitor and record vital Lf signs -the level of response, breathing, and pulse while waiting for tor help to arrive. Repeated doses of adrenaline (epinephrine) can be given at five-minute intervals if there is no improvement or the symptoms return.

Medical Conditions – FEVER
A sustained body temperature above the normal level of 37°c [98 6°F] is known as fever. It is usually caused by a bacterial or viral infection, but may be associated with earache, sore throat, measles, chickenpox, meningitis [opposite] or local infection, such as an abscess. The infection may have been acquired during overseas travel.
Moderate fever is not harmful to adults, but in young children a temperature above 37°C [98.6°F] can be dangerous and may trigger seizures. If you are in any doubt about a casualty’s condition, seek medical advice.
Symptoms and How to recognizes
- Raised body temperature above. 37°C (98 6°F)
- Pallor; casualty may feel cold with goose pimples, shivering, and chattering teeth.
Later:
- Hot, flushed skin and sweating.
- Headache.
What you can do:
- To bring down the fever.
- To obtain medical aid if necessary.
CAUTION
- If you are concerned about the casualty’s condition, seek medical advice.
- Do not over-or underdress a child with fever; do not sponge a child to cool her.
- Do not give aspirin to any person under 16 years of age.
To do:
- Keep casualty cool and comfortable -preferably in bed with a light covering.
2. Give her plenty of cool drinks to replace body fluids lost through sweating.

3. If the child appears distressed or unwell, she may have the recommended dose of paracetamol syrup (not aspirin). An adult may take the recommended dose of paracetamol tablets or her own painkillers.
4. Monitor and record a casualty’s vital signs -a level of response, breathing, pulse, and temperature until she recovers.
Special Causes – If a child become a very hot.

If there is a risk of seizure because of the raised temperature, cool the child further by removing his clothes and bed covering.
Medical Conditions – MENINGITIS
This is a condition during which the linings that surround the brain and therefore the medulla spinalis become inflamed It is often caused by bacteria or an epidemic and may affect any age bracket.
Meningitis is potentially a really serious illness and therefore the casualty may deteriorate very quickly. If you think of meningitis, you must seek urgent medical assistance as a prompt treatment in the hospital is significant. For this reason, it’s important that you simply are ready to recognize the symptoms of meningitis, which can include heat, headache, and a particular rash. With early diagnosis and treatment most, people make a full recovery.
Symptoms and How to recognizes
The symptoms and signs are usually not all present at the same time. They include:
- Flu-like illness with a high temperature.
- Cold hands and feet.
- Joint and limb pain
- Mottled or very pale skin.
- As the infection develops.
- Severe headache.
- Neck stiffness. (the casualty will not be able to touch her chest with her chin)
- Vomiting.
- Eyes become very sensitive to any light -daylight, electric light, or even the television.
- Drowsiness.
- In infants, there may also be high-pitched moaning or a whimpering cry, floppiness, and a tense or bulging fontanelle. (a soft part of the skull)
Later:
A distinctive rash of red or purple spots that do not fade when pressed.
To do:
- If a casualty’s condition is deteriorating, and you suspect meningitis, call 999/112 for emergency help even if she has already seen a doctor.

2. Seek urgent medical advice if you notice any of the signs of meningitis; for example, shielding eyes from the light. Do not wait for all the symptoms and signs to appear because they may not all develop. Treat the fever [opposite).

3. Check the casualty for signs of a rash. On dark skin, check on lighter parts of the body; for example, the inner eyelids or fingertips. If you see any signs, call 999/112 for emergency help.
4. While waiting for help 1 to arrive, reassure the casualty and keep her cool.
5. Monitor and record vital signs -level of response, breathing and pulse.
Important MENINGITIS rash
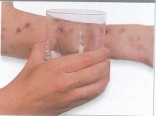
Accompanying the later stage of meningitis is a distinctive red or purple rash that does not fade if you press it. If you press the side of a glass firmly against most rashes they will fade; if a rash does not fade, call 999/112 for emergency help immediately.
Medical Conditions -HEADACHE

A headache may accompany any illness, particularly a feverish ailment such as flu. It may develop for no reason, but can often be traced to tiredness, tension, stress or undue heat, or cold. Mild “poisoning” caused by a stuffy or fume-filled atmosphere, or by excess alcohol or any other drug, can also induce a headache. However, a headache may also be the most prominent symptom of meningitis or a stroke.
Symptoms and How to recognizes
- To relieve the pain.
- To obtain medical advice if necessary.
CAUTION
- Do not give aspirin to anyone under 16 years of age.
- Seek urgent medical advice if the pain.
- Develops very suddenly.
- Is severe and incapacitating.
- Is accompanied by fever or vomiting.
- Is recurrent or persistent.
- Is accompanied by loss of strength or sensation. or by impaired consciousness.
- Is accompanied by a stiff neck and sensitivity to light.
- Follows a head injury.
To do:
- Help the casualty to sit or I lie down in a quiet place.

2. Give him a cold compress to hold against his head.
3. An adult may take the recommended dose of paracetamol tablets or his own painkillers. A child may have the recommended dose of paracetamol syrup. (not aspirin).
MIGRAINE

Migraine attacks are severe, “sickening” headaches and can be triggered by a variety of causes, such as allergy, stress, or tiredness Other triggers include lack of sleep, missed meals, alcohol, and some foods – for example, cheese or chocolate. Migraine sufferers usually know how to recognize and deal with attacks and may carry their own medication.
Symptoms and How to recognizes
- Before the attack, there may be a disturbance of vision in the form of flickering lights and/or a ·’ blind patch··.
- Intense throbbing headache. which is sometimes on just one side of the head.
- Abdominal pain, nausea, and vomiting.
- Inability to tolerate bright light or loud noise.
What you can do:
- To relieve the pain
- To obtain medical aid if necessary.
To do:
Help the casualty to take any medication I that he may have for migraine attacks.
Advise the casualty to lie down or sleep for a few hours in a quiet, dark room.
Provide him with some towels and a container in case he vomits.
If this is the first attack, advise the casualty to seek medical advice.
EARACHE AND TOOTHACHE

Earache can result from inflammation of the outer, middle, or inner ear, often caused by an infection associated with a cold, tonsillitis, or flu. It can also be caused by a boil, an object stuck in the ear canal, or transmitted pain from a tooth abscess. There may also be temporary hearing loss.
Earache often occurs when flying as a result of the changes in air pressure during ascent and descent. Infection can cause pus to collect in the middle ear; the eardrum may rupture, allowing the pus to drain, which temporarily eases the pain. Toothache can develop when the pulp inside a tooth becomes inflamed due to dental decay. If untreated, the pulp becomes infected, leading to an abscess, which causes throbbing pain. Infection may cause swelling around the tooth or jaw.
Your Aim:
- To relieve the pain.
- To obtain medical or dental advice if necessary.
CAUTION
- Do not give aspirin to anyone under 16 years of age.
- If there is a discharge from an ear, fever, or hearing loss, obtain medical help.
To Do:
An adult may take the recommended dose of paracetamol tablets or her own painkillers. A child may have the recommended dose of paracetamol syrup (not aspirin).
Give her a source of heat, such as a hot water bottle wrapped in a towel, to hold against the affected side of her face.
In addition for toothache you can soak a plug of cotton wool in oil of cloves to hold against the affected tooth.
Advise a casualty to seek medical advice if you are concerned, particularly if the casualty is a child. If a casualty has a toothache, advise her to see her dentist.
SORE THROAT
The most common sore throat is a “raw” feeling caused by inflammation, which is often the first sign of a cough or cold. Tonsillitis occurs when the tonsils at the back of the throat are infected. The tonsils become red and swollen and white spots of pus may be seen. Swallowing may be difficult and the glands at the angle of the jaw may be enlarged and sore.
Your Aim:
- To relieve the pain.
- To obtain medical advice if necessary.
CAUTION
- Do not give aspirin to anyone under 16 years of age.
- If you suspect tonsillitis, tell the casualty to seek medical advice.
To Do:
Give the casualty plenty of I fluids to help ease the pain and stop the throat from becoming dry.
An adult may take the recommended dose ofparacetamol tablets or his own painkillers. A child may have the recommended dose of paracetamol syrup (not aspirin).
ABDOMINAL PAIN
Pain in the abdomen often has a relatively minor cause, such as food poisoning. The pain of a stitch usually occurs during exercise and is sharp. Distension [widening] or obstruction of the intestine causes colic -pain that comes and goes in waves – which often makes the casualty double up in agony and may be accompanied by vomiting.
Occasionally abdominal pain is a sign of a serious disorder affecting the organs and other structures in the abdomen. If the appendix bursts or the intestine is damaged, the contents of the intestine can leak into the abdominal cavity, causing inflammation of the cavity lining. This life-threatening condition, called peritonitis, causes intense pain, which is made worse by movement or pressure on the abdomen, and will lead to shock.
An inflamed appendix [appendicitis] is especially common in children. Symptoms include pain [often starting in the center of the abdomen and moving to the lower right-hand side]. loss of appetite, nausea, vomiting, bad breath, and fever. If the appendix bursts, peritonitis will develop. The treatment is the urgent surgical removal of the appendix.
Your Aims:
- To relieve pain and discomfort.
- To obtain medical help if necessary.
CAUTION
If the pain is severe, or occurs with fever and vomiting, call 999/112 for emergency help. Treat the casualty for shock Do not give her medicine or allow her to eat or drink, because an anesthetic may be needed.
SPECIAL CASE STITCH
This common condition is a form of a cramp, usually associated with exercise, which occurs in the trunk or the sides of the chest. The most likely cause is a buildup in the muscles of chemical waste products, such as lactic acid, during physical exertion. Help the casualty to sit down and reassure him. The pain will usually ease quickly. If the pain does not disappear within a few minutes, or if you are concerned about the casualty’s condition, seek medical advice.
To Do:
Reassure the casualty and make her comfortable. Prop her up if she finds breathing difficult. Give her a container to use if she is vomiting.
Give the casualty a hot water bottle wrapped in a towel to hold against her abdomen. If in doubt about her condition, seek medical advice.
Medical Conditions – VOMITING AND DIARRHOEA
These problems are usually due to irritation of the digestive diarrhoea and vomiting can be caused by a number of different organisms, including viruses, bacteria, and parasites They usually result from eating contaminated food or drinking contaminated water, but infection can be passed directly from person to person Cleanliness and good hygiene help prevent infectious diarrhoea.
Vomiting and diarrhoea may occur either separately or and together salt Both conditions can cause the body to lose vital fluids s, resulting in dehydration. When they occur together, the risk of dehydration is increased and can be serious, especially in infants, young children and elderly people
The aim of treatment is to prevent dehydration by giving frequent sips of water or unsweetened fruit juice, even if the casualty is vomiting. Rehydration powder, which is added to water, provides the correct balance of water and salt to replace those lost through the vomiting and diarrhoea.
Symptoms and How to recognizes
- Nausea.
- Vomiting and later diarrhoea.
- Stomach pains.
- Fever.
Your Aim
- To reassure the casualty.
- To restore lost fluids and salts.
CAUTION
Do not give anti-diarrhea medicines.
If you are concerned about a casualty’s condition, particularly if the vomiting or diarrhoea is persistent, or the casualty is a young child or an older person, seek medical advice.
To Do:
Reassure the casualty if she is vomiting and give her a warm damp cloth to wipe her face.
Help her to sit down and when the vomiting stops give her water or unsweetened fruit juice to sip slowly and often.
When the casualty is hungry again, advise her to eat easily digested foods such as pasta, bread or potatoes for the first 24 hours.
Few things impact your life quite a significant ill health . Chronic diseases, including heart condition , stroke and diabetes; cancer; and communicable diseases affect the health of many people and price billions of dollars in medical expenses per annum in Missouri.
Lifestyle choices – like not smoking, maintaining a healthy weight, and being physically active – can help prevent a number of the foremost common chronic diseases and a few sorts of cancer. Regular health screenings can often discover chronic conditions and cancers early when treatment is more likely to achieve success. Communicable diseases can often be prevented through a variety of measures including vaccines and proper handwashing.
So making smart choices, Missourians can avoid or overcome many health problems and live longer and more productive lives.

